Free Advance Beneficiary Notice of Non-coverage PDF Form
Misconceptions
The Advance Beneficiary Notice of Non-coverage (ABN) form is often misunderstood, leading to confusion among patients and healthcare providers alike. Here are seven common misconceptions about the ABN form:
- The ABN is only for Medicare patients. Many believe that the ABN applies exclusively to Medicare beneficiaries. In reality, while it is primarily associated with Medicare, the concept can extend to other insurance programs that require similar notifications.
- Receiving an ABN means services will not be covered at all. Some patients think that if they receive an ABN, they will not receive coverage for the service. However, the ABN is meant to inform patients that a service may not be covered, allowing them to make an informed decision about whether to proceed.
- Signing an ABN means you are agreeing to pay for the service. Many individuals feel that signing the ABN obligates them to pay for the service. In truth, signing simply acknowledges that you understand the potential for non-coverage; it does not automatically mean you will be billed.
- The ABN must be signed before every service. It is a common belief that an ABN is required for every service provided. However, an ABN is only necessary when a provider believes that a service may not be covered by Medicare or other insurers.
- Providers are required to issue an ABN for all non-covered services. Some think that healthcare providers must issue an ABN for every service that could potentially be denied. However, it is at the provider's discretion to issue an ABN based on their judgment of coverage likelihood.
- All services listed on an ABN are automatically denied. Patients often assume that any service mentioned on an ABN will definitely not be covered. This is misleading, as the ABN is a precautionary measure, and coverage decisions are ultimately made by the insurance provider.
- Once you sign an ABN, you cannot appeal the decision. There is a misconception that signing an ABN waives your right to appeal. In fact, patients can still appeal coverage decisions even after signing an ABN, as it does not affect their right to challenge a denial.
Understanding these misconceptions can empower patients to navigate their healthcare options more effectively. Knowledge is crucial when it comes to making informed decisions about medical services and potential costs.
Documents used along the form
The Advance Beneficiary Notice of Non-coverage (ABN) form is an important document in the healthcare system, particularly in the context of Medicare. It informs patients when a service may not be covered, allowing them to make informed decisions about their care. Several other forms and documents are often used in conjunction with the ABN to ensure clarity and compliance in the billing and reimbursement process. Below is a list of these related documents.
- Medicare Summary Notice (MSN): This document is sent to beneficiaries every three months and summarizes the services received, the amounts billed, and what Medicare has paid. It helps patients understand their costs and coverage.
- Detailed Explanation of Non-Coverage (DENC): This form provides a detailed account of why a service was not covered by Medicare. It outlines the specific reasons for non-coverage and can help patients appeal decisions if they believe a service should be covered.
- Claim Form (CMS-1500): This form is used by healthcare providers to bill Medicare for services rendered. It includes details about the patient, the provider, and the services provided, and is essential for processing claims.
- Motorcycle Bill of Sale: This essential document facilitates the transfer of motorcycle ownership, ensuring clarity in the transaction. For an online version, you can find the form at PDF Documents Hub.
- Patient Authorization Form: This document allows healthcare providers to share a patient’s medical information with other parties, such as insurers or family members. It ensures that patient privacy is respected while facilitating communication about care and coverage.
These documents collectively support the transparency and efficiency of the healthcare billing process. Understanding each form's purpose can empower patients to navigate their healthcare options more effectively.
Check out Popular Documents
Family Law Financial Affidavit Short Form Florida - The affidavit can also serve as a reference point for future financial assessments.
Wage and Tax Statement - Employers contribute to unemployment insurance, which is reflected in the W-2.
For those seeking to grasp the significance of the Hold Harmless Agreement, understanding its role in legal contexts is crucial. This important document, often employed in various situations to mitigate liability risks, can be further explored through our resource on the complete Hold Harmless Agreement guide.
Free Printable Five Wishes Pdf - Five Wishes is accessible to anyone aged 18 and older, making it a vital tool for all adults.
Key Details about Advance Beneficiary Notice of Non-coverage
What is the Advance Beneficiary Notice of Non-coverage (ABN)?
The Advance Beneficiary Notice of Non-coverage, commonly known as the ABN, is a form that Medicare providers use to inform beneficiaries that a service or item may not be covered by Medicare. This notice is essential because it allows you to make informed decisions about your healthcare. If you receive an ABN, it means the provider believes that Medicare may not pay for the service, and you may be responsible for the costs.
When should I receive an ABN?
You should receive an ABN before a service is provided, especially if the provider thinks that Medicare might deny coverage. This could happen in situations where the service is not deemed medically necessary, or if it’s considered experimental. The provider must give you the ABN in advance, allowing you to understand your potential financial responsibility before proceeding.
What should I do if I receive an ABN?
If you receive an ABN, take a moment to review it carefully. Here are some steps to consider:
- Read the notice thoroughly to understand why the service may not be covered.
- Decide whether you want to proceed with the service, knowing you might have to pay out-of-pocket.
- If you have questions, don’t hesitate to ask your healthcare provider for clarification.
- Keep a copy of the ABN for your records, especially if you choose to go ahead with the service.
What happens if I don’t receive an ABN for a service that isn’t covered?
If you do not receive an ABN and Medicare denies coverage for a service, you may be able to appeal the decision. However, without an ABN, it can be more challenging to argue that you were not informed about the potential costs. Therefore, it’s crucial to ensure you receive an ABN whenever there’s a possibility of non-coverage.
Can I appeal a denial if I signed an ABN?
Is there a specific format for the ABN?
Similar forms
- Medicare Summary Notice (MSN): This document provides beneficiaries with a summary of services received, the costs incurred, and the amount covered by Medicare. Like the Advance Beneficiary Notice of Non-coverage (ABN), it informs beneficiaries about their financial responsibilities for services rendered.
- Hold Harmless Agreement: This legal document ensures that one party will not hold the other liable for any risks or losses, similar to the functions of the aforementioned documents. For more information on how to fill out this agreement, visit https://texasformspdf.com/fillable-hold-harmless-agreement-online/.
- Notice of Exclusion from Medicare Benefits (NEMB): This notice is issued when a service is not covered by Medicare. Similar to the ABN, it alerts beneficiaries that they may be responsible for payment, clarifying the limits of coverage.
- Patient Responsibility Notice: This document outlines the patient's financial obligations for services provided. It parallels the ABN by emphasizing the potential out-of-pocket costs associated with certain treatments or procedures.
- Prior Authorization Request: This form is used to obtain approval from Medicare before a service is rendered. Like the ABN, it seeks to clarify coverage issues and the financial implications of care decisions.
- Explanation of Benefits (EOB): After a claim is processed, this document explains what services were covered and what costs the patient must pay. It shares similarities with the ABN in that it informs beneficiaries of their financial responsibilities.
- Claim Denial Letter: When a claim is denied, this letter explains the reasons for the denial. It is akin to the ABN in that it communicates important coverage information to beneficiaries, often leading to potential out-of-pocket costs.
- Out-of-Pocket Cost Estimate: This document provides an estimate of the costs a patient may incur for a specific service. Similar to the ABN, it helps beneficiaries understand their financial responsibilities ahead of receiving care.
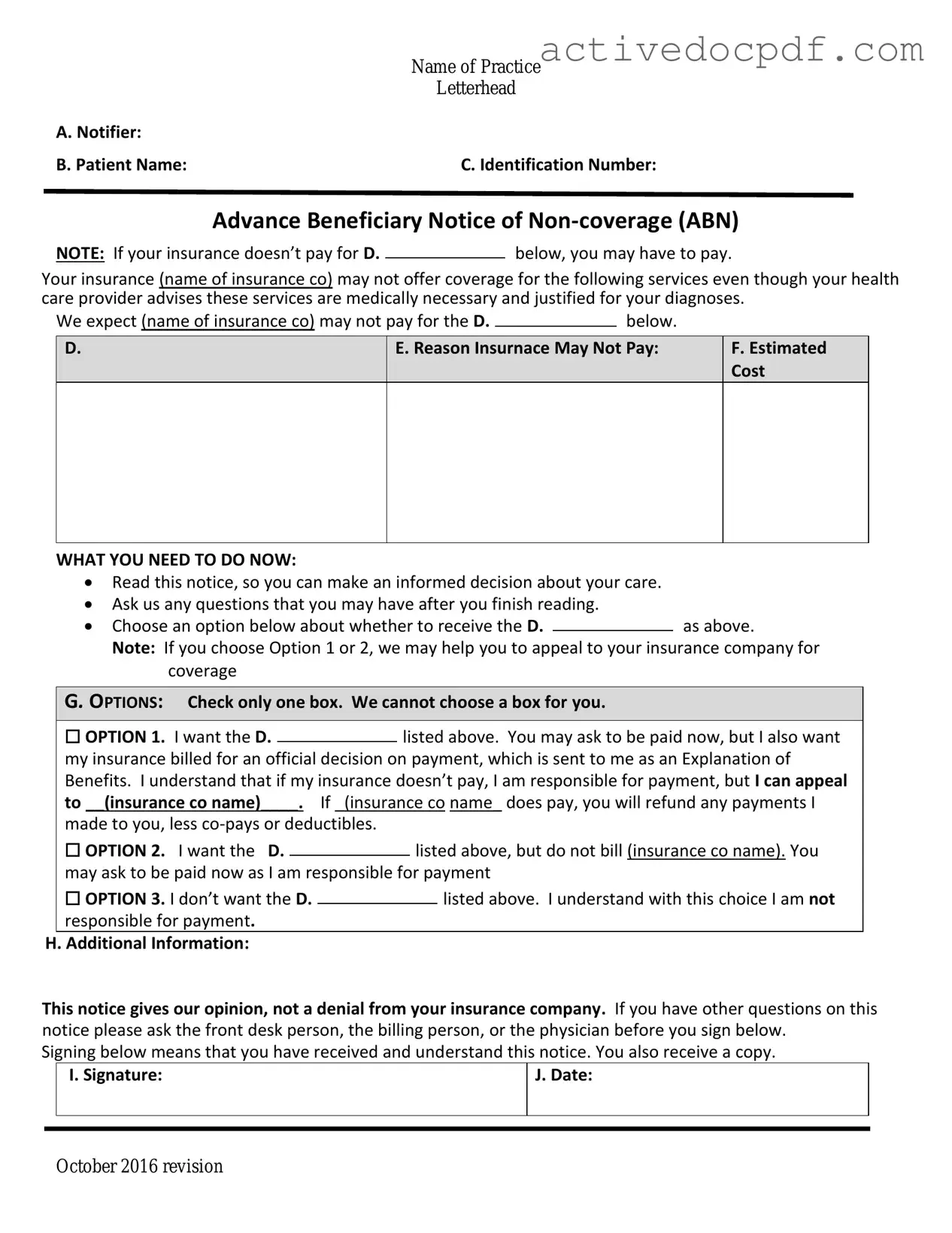
Guide to Filling Out Advance Beneficiary Notice of Non-coverage
After receiving the Advance Beneficiary Notice of Non-coverage form, it’s important to complete it accurately. This form helps clarify the services you may receive and the potential costs involved. Follow the steps below to ensure you fill it out correctly.
- Start with the date at the top of the form. Write the date when you are filling out the form.
- In the section for patient information, provide your full name, address, and Medicare number.
- Next, indicate the specific service or item that is being discussed. Clearly describe what you are receiving or what was proposed.
- In the section for the reason for non-coverage, check the box that applies to your situation. This could include reasons like the service being not medically necessary.
- Sign and date the form in the designated area. This confirms that you understand the information provided.
- Make a copy of the completed form for your records before submitting it to your healthcare provider.
Once you have completed the form, submit it to your healthcare provider. They will review it and inform you of any next steps regarding your coverage and potential costs.