Free Annual Physical Examination PDF Form
Misconceptions
Misconceptions about the Annual Physical Examination form can lead to confusion and incomplete submissions. Here are seven common misconceptions along with clarifications:
- It is optional to complete the form. Many believe that filling out the Annual Physical Examination form is not necessary. In reality, providing complete information is essential to ensure a thorough medical evaluation.
- Only new patients need to fill it out. Some think that only first-time patients must complete the form. However, all patients, regardless of their history, should fill it out to provide the most current health information.
- Medications do not need to be listed if they are not changed. Individuals may think that if their medications remain the same, they do not need to list them. It is important to include all current medications, even if there are no changes, to give a complete picture of health.
- Allergies and sensitivities are optional information. Some may believe that they can skip this section. However, detailing allergies and sensitivities is crucial for safe medical treatment and avoiding adverse reactions.
- The form can be filled out during the appointment. There is a misconception that the form can be completed in the waiting room. It is best to fill it out beforehand to avoid delays and ensure all information is accurate.
- Only physical health issues need to be reported. Some individuals think that only physical conditions are relevant. However, mental health and emotional well-being are also important and should be included in the medical history.
- The form is only for adults. Many assume that the Annual Physical Examination form is only for adults. In fact, it is applicable for individuals of all ages, including children, who require a physical examination.
Documents used along the form
The Annual Physical Examination form is a vital document that helps healthcare providers assess an individual's overall health. Alongside this form, several other documents often accompany it to ensure a comprehensive understanding of a patient’s medical history and current health status. Below is a list of commonly used forms and documents that complement the Annual Physical Examination form.
- Medical History Questionnaire: This form collects detailed information about the patient's past medical conditions, surgeries, allergies, and family health history. It provides context for the healthcare provider to make informed decisions during the examination.
- Immunization Record: This document lists all vaccinations the patient has received, including dates and types. It is crucial for tracking immunization status and ensuring the patient is up to date on necessary vaccines.
- Medication List: A comprehensive list of all medications the patient is currently taking, including dosages and frequencies. This helps avoid potential drug interactions and ensures the provider is aware of all treatments the patient is undergoing.
- Lab Test Results: This includes results from any recent blood tests, urinalysis, or other diagnostic tests. Having these results on hand allows the provider to assess the patient’s health more effectively during the examination.
- Referral Forms: If the patient needs to see a specialist, this form outlines the reason for the referral and any pertinent medical information. It streamlines the process of obtaining specialized care.
- Rental Application Form: Before signing a lease, landlords often require a rental application to evaluate potential tenants. This critical document can be found at nyforms.com/rental-application-template/ and plays a vital role in establishing a strong landlord-tenant relationship.
- Patient Consent Form: This document ensures that the patient understands and agrees to the examination and any procedures that may be performed. It protects both the patient’s rights and the provider’s responsibilities.
These documents work together to create a holistic view of a patient’s health, facilitating better care and more informed medical decisions. By ensuring that all necessary forms are completed and available, healthcare providers can optimize the examination process and enhance patient outcomes.
Check out Popular Documents
Parent Consent Letter for Travel - It demonstrates compliance with safety and travel guidelines for youth.
Crest of Arms - A design that highlights environmental stewardship.
For more information on how to correctly file and manage your IRS Form 2553, resources are available at PDF Documents Hub, which offers guidance that can streamline the process and ensure compliance with tax regulations.
Ncoer Signing Order - The form aims to foster transparent communication regarding performance between NCOs and their raters.
Key Details about Annual Physical Examination
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form serves as a comprehensive tool for gathering essential health information prior to a medical appointment. By collecting details about medical history, current medications, immunizations, and any significant health conditions, the form helps healthcare providers assess an individual's overall health and tailor their care accordingly. Completing this form accurately can lead to more effective and efficient medical evaluations.
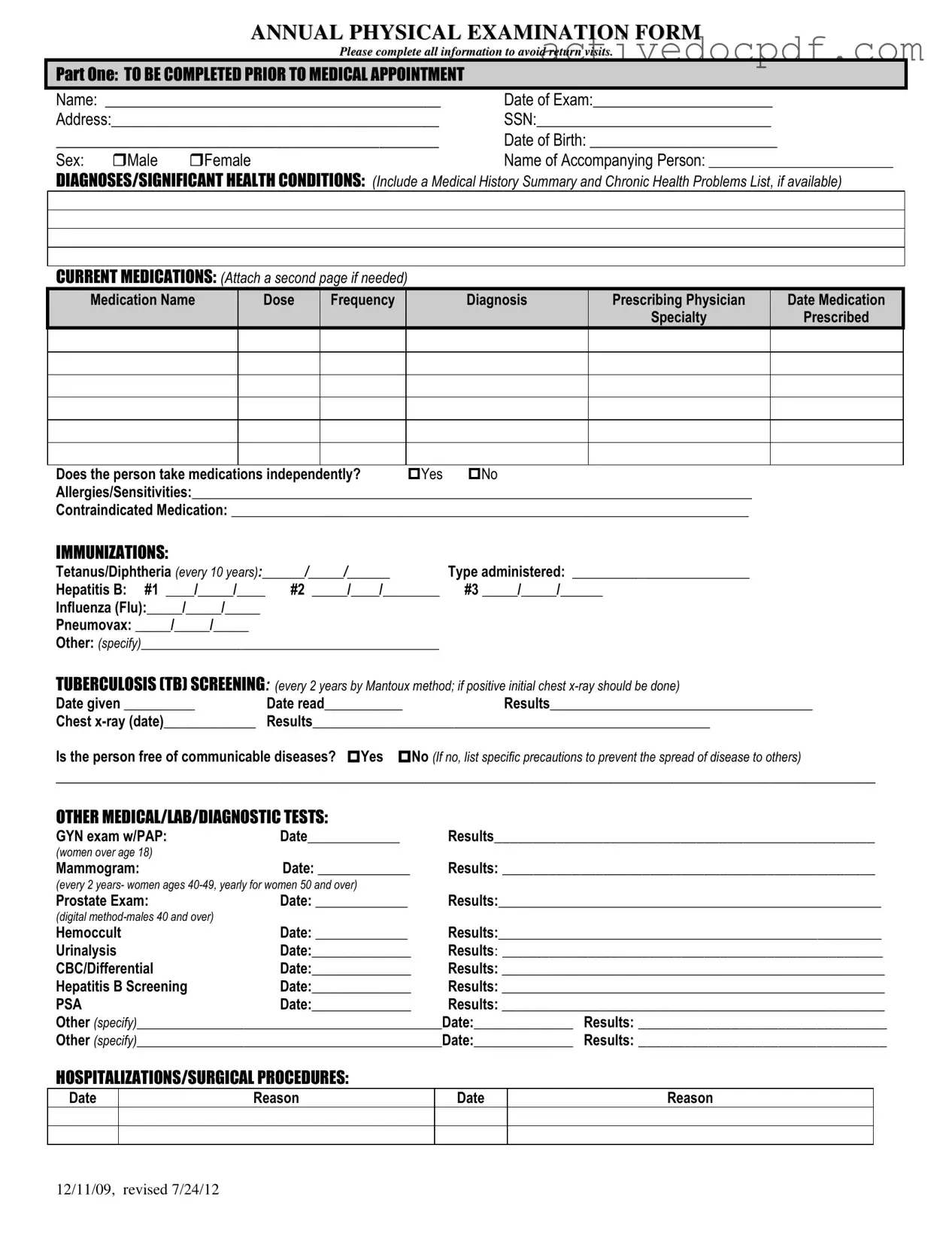
What information is required in Part One of the form?
Part One of the form requires personal information such as the individual's name, date of birth, and address. Additionally, it asks for the Social Security Number and details about any accompanying person. Medical history is crucial here; individuals must list diagnoses, chronic health problems, current medications, allergies, and any contraindicated medications. Immunization records and tuberculosis screening information are also included to ensure comprehensive health assessment.
How should I prepare for filling out the form?
Preparation for filling out the form involves gathering relevant health documents and records. Individuals should review their medical history, including past diagnoses, surgeries, and hospitalizations. It is also advisable to compile a list of current medications, including dosages and prescribing physicians. If available, immunization records should be collected to provide accurate dates and types of vaccines received. This preparation will help ensure that all necessary information is included, minimizing the need for follow-up visits.
What if I have allergies or sensitivities?
If an individual has allergies or sensitivities, it is vital to document them clearly on the form. This information helps healthcare providers avoid prescribing medications or treatments that could trigger an allergic reaction. Including specific details about the nature of the allergies, such as severity and past reactions, can enhance patient safety and inform future medical decisions.
What tests are included in the Annual Physical Examination?
The Annual Physical Examination may include a variety of tests, depending on age, gender, and individual health needs. Common tests include blood pressure measurements, urinalysis, and screenings for various conditions like prostate health for men and mammograms for women. Additional tests may be recommended based on medical history or findings during the examination. It is essential for individuals to discuss any specific concerns with their healthcare provider during the appointment.
What happens if I have a change in health status from the previous year?
If there has been a change in health status, it is crucial to indicate this on the form. This information can guide the healthcare provider in adjusting care plans, recommending further tests, or making referrals to specialists. It is important to provide specific details about the changes, as they can significantly impact overall health and treatment strategies.
How will my information be used and protected?
The information collected through the Annual Physical Examination form is used solely for the purpose of providing medical care and improving health outcomes. Healthcare providers are bound by confidentiality laws, ensuring that personal health information is protected. Individuals should feel secure knowing that their data will be handled with the utmost care and only shared with authorized personnel involved in their treatment.
Similar forms
-
Medical History Form: This document collects a patient’s past health information, including previous illnesses, surgeries, and family health history. Like the Annual Physical Examination form, it aims to provide a comprehensive view of a patient’s health for better diagnosis and treatment planning.
- Gift Declaration Form: Similar to the Annual Physical Examination form, the Gift Declaration Form confirms the transfer of ownership of an item without expectation of payment. This is crucial for ensuring compliance with legal requirements when gifting a vehicle, and you can fill out the necessary details through this link: https://texasformspdf.com/fillable-affidavit-of-gift-online/.
-
Medication List: This document details all medications a patient is currently taking, including dosages and prescribing physicians. Similar to the Annual Physical Examination form, it ensures that healthcare providers are aware of potential drug interactions and allergies.
-
Immunization Record: This document tracks vaccinations a patient has received over their lifetime. Like the immunization section in the Annual Physical Examination form, it helps ensure that patients are up-to-date on necessary vaccines to prevent disease.
-
Lab Test Results: This document presents the outcomes of various diagnostic tests performed on a patient. It parallels the Annual Physical Examination form by summarizing important health metrics that aid in monitoring and managing a patient’s health.
-
Referral Form: This document is used when a primary care physician refers a patient to a specialist. Like the recommendations section in the Annual Physical Examination form, it helps coordinate care and ensures that all relevant health information is shared.
-
Physical Therapy Evaluation: This document assesses a patient’s physical capabilities and rehabilitation needs. Similar to the evaluation sections in the Annual Physical Examination form, it focuses on the patient’s physical health and any necessary interventions.
-
Health Risk Assessment: This document evaluates a patient’s risk factors for various diseases. Like the health maintenance recommendations in the Annual Physical Examination form, it aims to identify areas for improvement in a patient’s lifestyle.
-
Emergency Contact Form: This document lists individuals to contact in case of a medical emergency. Similar to the information pertinent to diagnosis and treatment section in the Annual Physical Examination form, it ensures that critical health information is accessible during emergencies.
-
Patient Consent Form: This document secures a patient’s permission for treatment and sharing of their medical information. Like the signature section in the Annual Physical Examination form, it confirms that the patient agrees to the proposed care plan.
Guide to Filling Out Annual Physical Examination
Completing the Annual Physical Examination form is an important step in ensuring your health needs are addressed. After filling out the form, you will be able to present it to your healthcare provider at your appointment. This will help facilitate a thorough examination and discussion of your medical history.
- Personal Information: Fill in your name, date of exam, address, Social Security Number (SSN), date of birth, and sex (male or female).
- Accompanying Person: Provide the name of the person accompanying you to the appointment.
- Medical History: List any diagnoses or significant health conditions. Include a summary of your medical history and any chronic health problems if available.
- Current Medications: Write down all medications you are currently taking. Include the medication name, dose, frequency, diagnosis, prescribing physician, date prescribed, and specialty of the prescribing physician. Indicate if you take medications independently.
- Allergies: List any allergies or sensitivities you have, as well as any contraindicated medications.
- Immunizations: Fill in the dates and types of immunizations received, including Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax.
- TB Screening: Provide the date the TB test was given, the date it was read, and the results. Include details of any chest x-ray if applicable.
- Communicable Diseases: Indicate if you are free of communicable diseases. If not, list precautions to prevent the spread of disease.
- Medical Tests: Record any other medical, lab, or diagnostic tests you have had, including GYN exams, mammograms, prostate exams, and any other relevant tests.
- Hospitalizations/Surgical Procedures: List any hospitalizations or surgical procedures, including dates and reasons.
- General Physical Examination: Fill in your blood pressure, pulse, respirations, temperature, height, and weight.
- Evaluation of Systems: For each system listed (e.g., eyes, ears, lungs), indicate if normal findings were observed and provide comments if necessary.
- Vision and Hearing Screening: Note if further evaluation is recommended for vision and hearing.
- Additional Comments: Include any additional comments, medical history reviews, medication changes, recommendations for health maintenance, and any special instructions.
- Limitations or Restrictions: Indicate if there are any limitations or restrictions for activities and whether you use adaptive equipment.
- Change in Health Status: Specify if there has been any change in health status from the previous year.
- Physician Information: At the end of the form, the physician must print their name, sign, and date the form. Include the physician's address and phone number.