Free Cna Shower Sheets PDF Form
Misconceptions
Misconceptions about the CNA Shower Sheets form can lead to misunderstandings in its purpose and use. Here are ten common misconceptions, clarified for better understanding:
- The form is only for recording skin issues. Many believe the CNA Shower Sheets are solely for documenting skin abnormalities. In reality, the form also includes areas for assessing overall resident care, including toenail maintenance.
- Only serious skin problems need to be reported. Some think that only severe issues like deep wounds or infections require reporting. However, all abnormalities, even minor ones like dryness or scratches, should be documented and communicated.
- The form is optional for CNAs. There is a misconception that using the form is not mandatory. In fact, completing the CNA Shower Sheets is an essential part of providing thorough care and ensuring proper communication with nursing staff.
- Only the charge nurse can assess skin conditions. Many assume that only the charge nurse is responsible for skin assessments. In truth, CNAs are trained to perform these assessments and must report their findings promptly.
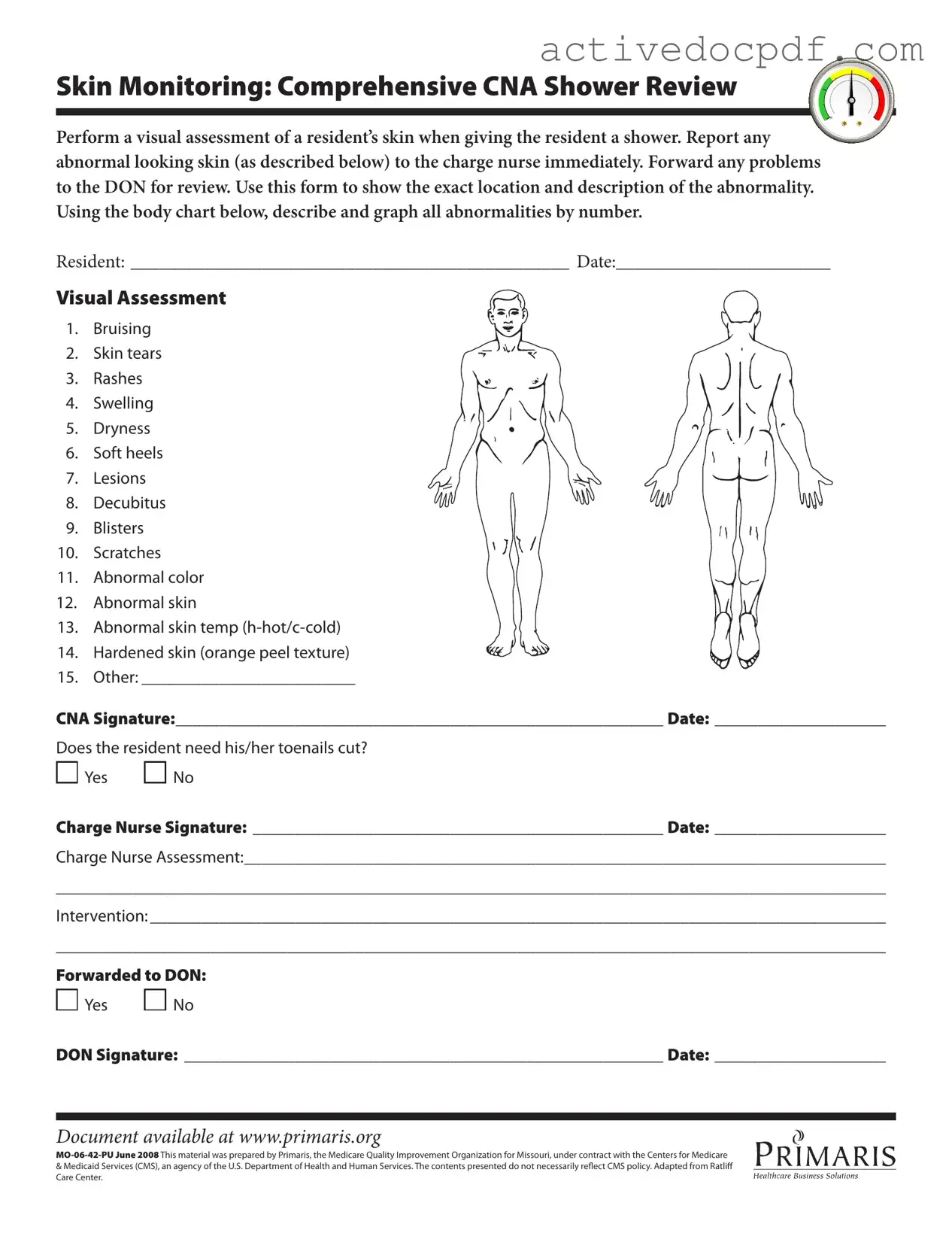
- The body chart is not important. Some may overlook the body chart included in the form. This chart is crucial for accurately documenting the location of skin abnormalities, which aids in tracking changes over time.
- Documentation is only needed if there is a problem. A common belief is that documentation is unnecessary if everything appears normal. Regular documentation helps establish a baseline for each resident’s skin condition, which is valuable for future assessments.
- The form is not reviewed by higher management. Some think that once the form is completed, it stays with the CNA. In fact, it is forwarded to the Director of Nursing (DON) for further review, ensuring comprehensive oversight.
- Skin assessments are only done during showers. There is a misconception that skin assessments are limited to shower times. Skin evaluations should be conducted regularly, regardless of bathing schedules, to ensure ongoing monitoring.
- All abnormalities require immediate intervention. Some may believe that every abnormal finding necessitates immediate action. While reporting is essential, the charge nurse will determine the appropriate intervention based on the assessment.
- The CNA Shower Sheets are outdated. Some individuals think the form is no longer relevant. However, it remains a critical tool for documenting skin health and ensuring quality care in nursing facilities.
Documents used along the form
The CNA Shower Sheets form is an essential document used in healthcare settings to monitor residents' skin during showers. It is often accompanied by various other forms and documents that help ensure comprehensive care and proper documentation. Below is a list of related documents that may be utilized alongside the CNA Shower Sheets.
- Resident Care Plan: This document outlines the specific needs and preferences of each resident, including their medical history, treatment goals, and any required interventions.
- Incident Report: Used to document any unexpected events or accidents involving a resident. This report helps track incidents and ensure appropriate follow-up actions are taken.
- Power of Attorney: This critical document allows individuals to assign decision-making authority to an agent, which is particularly important for financial and healthcare matters. For more information, visit https://documentonline.org.
- Skin Assessment Form: This form provides a detailed evaluation of a resident's skin condition over time, allowing staff to monitor changes and identify potential issues early.
- Daily Progress Notes: These notes are completed by caregivers to provide updates on a resident's condition and any changes in their care needs or behaviors.
- Nursing Assessment Form: A comprehensive assessment tool that gathers vital information about a resident's physical and mental health, ensuring all aspects of their care are considered.
- Medication Administration Record (MAR): This record tracks all medications given to a resident, including dosages and times, ensuring proper medication management.
- Fall Risk Assessment: This document evaluates a resident's risk of falling and outlines necessary precautions or interventions to minimize that risk.
- Personal Hygiene Record: This form tracks the frequency and type of personal hygiene activities performed for each resident, ensuring their dignity and cleanliness are maintained.
- Transfer/Discharge Summary: This document summarizes a resident's care and condition upon transfer or discharge, ensuring continuity of care as they move to a new setting.
Each of these forms plays a vital role in delivering quality care and maintaining accurate records. Together, they support the overall health and well-being of residents, ensuring that their needs are met effectively and compassionately.
Check out Popular Documents
Direct Deposit Authorization Form - Contact your bank to confirm that they accept direct deposits.
How Do You Renew Your Passport - Use the website for travel advice before planning any trips abroad.
For those looking to create a comprehensive and legally binding Bill of Sale, utilizing resources like PDF Documents Hub can be immensely helpful in ensuring all necessary information is accurately documented, safeguarding both parties in the transaction.
Broward Animal Control - Information about the vaccine's manufacturer and serial number is crucial for tracking.
Key Details about Cna Shower Sheets
What is the purpose of the CNA Shower Sheets form?
The CNA Shower Sheets form is designed to help Certified Nursing Assistants (CNAs) conduct thorough skin assessments while giving residents a shower. It serves as a record of any abnormalities found on the resident’s skin, such as bruises, rashes, or lesions. By documenting these findings, CNAs can ensure that any issues are reported to the charge nurse and addressed promptly, promoting the overall health and well-being of the residents.
How should I fill out the visual assessment section?
When filling out the visual assessment section, carefully examine the resident’s skin during the shower. Look for specific abnormalities listed on the form, such as bruising, swelling, or dryness. For each abnormality you observe, mark its location on the body chart provided and describe it in detail. Be thorough in your descriptions to ensure that the charge nurse has all the information needed for further assessment.
What steps should I take if I notice an abnormality?
If you notice any abnormality during the skin assessment, you should report it to the charge nurse immediately. This ensures that the issue is addressed quickly. After reporting, document the abnormality on the form, including its location and description. The charge nurse will then assess the situation and determine if further action is necessary, such as forwarding the issue to the Director of Nursing (DON).
What should I do if the resident needs their toenails cut?
If the resident requires a toenail trim, you should indicate this on the form by checking "Yes" in the designated section. This information will be passed along to the charge nurse, who will decide on the appropriate intervention. Proper foot care is essential for residents, especially those with limited mobility or health issues that affect their feet.
How is this form utilized in the overall care process?
The CNA Shower Sheets form is an important tool in the overall care process. It facilitates communication between CNAs, charge nurses, and the Director of Nursing. By documenting skin assessments and any necessary interventions, the form helps ensure that residents receive timely and appropriate care. This collaborative approach enhances the quality of care provided and supports the health and safety of all residents.
Similar forms
- Patient Assessment Form: Similar to the CNA Shower Sheets, this form is used to evaluate a patient's overall health status. It includes sections for documenting vital signs, physical examinations, and any notable changes in the patient's condition.
- Skin Assessment Tool: This document focuses specifically on the evaluation of skin integrity. Like the CNA Shower Sheets, it allows healthcare providers to record findings related to skin conditions, including rashes, lesions, and other abnormalities.
-
Rental Application Form: This essential document helps landlords evaluate potential tenants with comprehensive information, ensuring a good fit for the property. For more details, visit https://nyforms.com/rental-application-template/.
- Incident Report Form: This form is used to document any unexpected events or accidents involving a patient. It serves a similar purpose in recording details about a specific incident, including observations and actions taken, much like the reporting of skin abnormalities.
- Care Plan Template: This document outlines the strategies and interventions for a patient’s care. It parallels the CNA Shower Sheets in that it requires input from various healthcare providers to ensure a comprehensive approach to patient needs.
- Daily Progress Notes: These notes are used to track a patient’s condition on a daily basis. They share a common goal with the CNA Shower Sheets of providing ongoing documentation of a patient’s health and any changes that occur.
- Fall Risk Assessment: This form evaluates a patient's risk of falling and includes observations similar to those found in the CNA Shower Sheets. It requires careful observation and documentation of risk factors, just as skin abnormalities are recorded.
- Medication Administration Record (MAR): This record tracks medications given to patients. While it focuses on medications rather than skin assessments, it shares the importance of accurate documentation and timely reporting of any issues.
- Vital Signs Record: This document is used to log a patient’s vital signs over time. Like the CNA Shower Sheets, it serves as a crucial tool for monitoring changes in a patient’s condition.
- Wound Care Documentation: This form is specifically for documenting the care and assessment of wounds. It is similar to the CNA Shower Sheets in that it requires detailed descriptions and observations about the wound's condition and any interventions performed.
- Patient Transfer Form: This document is used when transferring a patient between departments or facilities. It includes a summary of the patient's condition and care needs, similar to how the CNA Shower Sheets summarize skin assessments.
Guide to Filling Out Cna Shower Sheets
Completing the CNA Shower Sheets form is an essential part of documenting a resident's skin condition during their shower. Accurate and thorough completion of this form ensures that any abnormalities are reported and addressed promptly. Follow the steps below to fill out the form correctly.
- Begin by writing the resident's name in the designated space labeled RESIDENT:.
- Next, enter the current date in the space labeled DATE:.
- Perform a visual assessment of the resident's skin while giving the shower.
- Identify any abnormalities from the list provided. Mark each abnormality on the body chart by number. The options include:
- 1. Bruising
- 2. Skin tears
- 3. Rashes
- 4. Swelling
- 5. Dryness
- 6. Soft heels
- 7. Lesions
- 8. Decubitus
- 9. Blisters
- 10. Scratches
- 11. Abnormal color
- 12. Abnormal skin
- 13. Abnormal skin temperature (h-hot/c-cold)
- 14. Hardened skin (orange peel texture)
- 15. Other: _________________________
- After documenting the abnormalities, sign your name in the space labeled CNA Signature:.
- Enter the date of the assessment in the space labeled Date: below your signature.
- Indicate whether the resident needs their toenails cut by checking either Yes or No.
- The charge nurse should then sign the form in the space labeled Charge Nurse Signature:.
- Enter the date of the charge nurse's assessment in the space labeled Date:.
- Provide a detailed assessment in the Charge Nurse Assessment: section.
- Document any interventions in the Intervention: section.
- Finally, indicate whether the form has been forwarded to the Director of Nursing (DON) by checking Yes or No.
- The DON should sign the form in the space labeled DON Signature:.
- Enter the date of the DON's signature in the space labeled Date:.