Free Medication Administration Record Sheet PDF Form
Misconceptions
Understanding the Medication Administration Record Sheet (MARS) is crucial for ensuring proper medication management. However, several misconceptions can lead to confusion. Here are eight common misunderstandings:
- It's only for nurses. Many believe that only nurses can fill out the MARS. In reality, anyone responsible for administering medication, including caregivers and aides, can use this form.
- It’s optional. Some think using the MARS is optional. In fact, it is often a required part of medication management to ensure accurate records and accountability.
- One form works for all patients. Many assume a single MARS can be used for all patients. Each patient should have their own individualized MARS to accurately reflect their specific medication needs.
- It’s only for prescription medications. Some people believe the MARS is only for prescription drugs. However, it can also be used for over-the-counter medications and supplements.
- Recording is only necessary if there’s a change. Many think they only need to record changes in medication. In truth, every administration must be documented to maintain an accurate record.
- Refusals don’t need to be noted. Some believe that if a patient refuses medication, it doesn’t need to be recorded. However, refusals should always be documented to track patient compliance and inform healthcare decisions.
- Only the person administering medication needs to fill it out. There is a misconception that only the administrator should complete the MARS. In reality, it’s important for other healthcare team members to review and update the form as necessary.
- It’s not important to check the time of administration. Some think the exact time of medication administration is not critical. However, timing can significantly impact the effectiveness of the medication and patient safety.
By addressing these misconceptions, individuals can better understand the importance of the Medication Administration Record Sheet and its role in patient care.
Documents used along the form
The Medication Administration Record Sheet is a vital document used to track the administration of medications to consumers. It ensures that medications are given at the correct times and helps maintain a clear record of any changes or refusals. Several other forms and documents complement this record, enhancing the overall medication management process.
- Medication Order Form: This form details the specific medications prescribed by a physician. It includes dosage, frequency, and duration, serving as the primary instruction for medication administration.
- Articles of Incorporation Form: To establish a corporation legally, refer to our essentials of Articles of Incorporation filing for guidance on necessary details and compliance.
- Patient Consent Form: This document confirms that the patient or their guardian has agreed to the medication regimen. It outlines potential risks and benefits, ensuring informed consent is obtained.
- Medication Reconciliation Form: Used during transitions of care, this form compares the patient’s current medications with those being prescribed. It helps identify discrepancies and prevent medication errors.
- Adverse Drug Reaction Report: This form is completed when a patient experiences an unexpected side effect from a medication. It documents the reaction and is essential for monitoring patient safety.
- Medication Disposal Record: This document tracks the proper disposal of unused or expired medications. It ensures compliance with safety regulations and helps prevent accidental ingestion.
- Daily Progress Notes: These notes provide a summary of the patient's health status and any changes in their condition. They may include observations related to medication effects and overall well-being.
These forms work together to create a comprehensive system for managing medications effectively. Each document plays a critical role in ensuring patient safety and adherence to prescribed treatments.
Check out Popular Documents
Pharmacy Dispensing Labels - Includes a barcode for pharmacy tracking purposes.
To facilitate a smooth transaction, using the New York Trailer Bill of Sale is highly recommended, as it provides all necessary information about the sale, including the purchase price and trailer specifics. For those looking for a template to ensure they include all essential details, you can find a useful resource at https://nyforms.com/trailer-bill-of-sale-template.
Automation in Business Credit - Help us understand your business by filling out this credit application.
Stock Transfer Forms - The form supports easy identification of stockholder rights and privileges.
Key Details about Medication Administration Record Sheet
What is the purpose of the Medication Administration Record Sheet?
The Medication Administration Record Sheet (MARS) is designed to track the administration of medications to consumers. It helps ensure that individuals receive their prescribed medications at the right times and in the correct dosages. This form serves as a vital communication tool among healthcare providers, caregivers, and family members.
Who should use the Medication Administration Record Sheet?
This form is primarily used by healthcare providers, including nurses, caregivers, and other staff responsible for administering medications. Additionally, family members who are involved in the care of an individual may find it useful to monitor medication adherence.
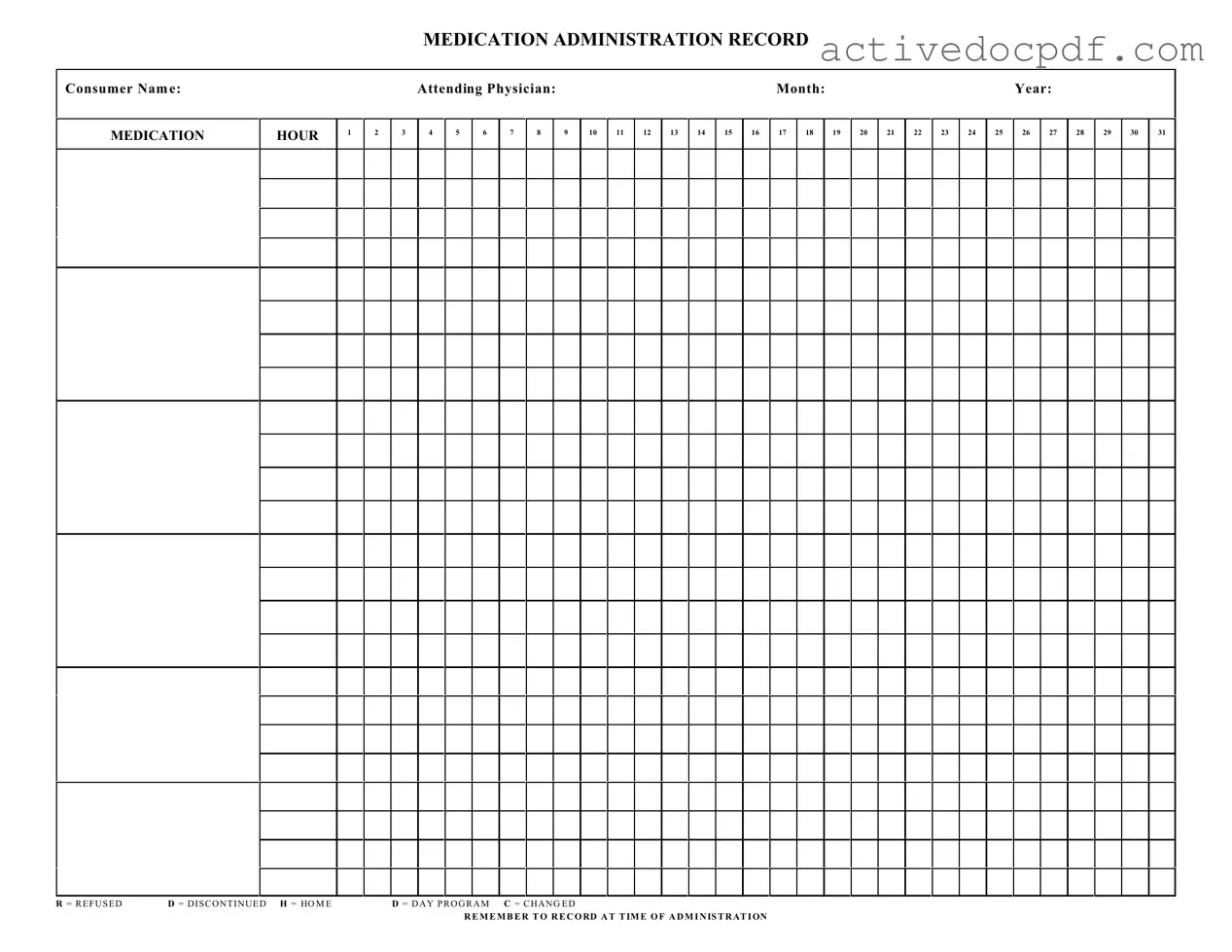
How is the Medication Administration Record Sheet structured?
The MARS is organized by consumer name and includes sections for the attending physician, month, and year. It features a grid with hours listed across the top and space for medication entries. Symbols such as R (Refused), D (Discontinued), H (Home), D (Day Program), and C (Changed) are included to indicate the status of medication administration.
What information needs to be recorded on the MARS?
It is important to record the following information on the MARS:
- The name of the consumer receiving the medication.
- The name of the attending physician.
- The specific month and year.
- The time of administration for each medication.
- Any refusals, changes, or discontinuations of medication.
How should medications be documented on the MARS?
Medications should be documented by entering the medication name and dosage in the appropriate time slot. It's crucial to check off the corresponding box to indicate whether the medication was administered, refused, or discontinued. Accurate and timely documentation is essential for maintaining a complete medication history.
What should be done if a medication is refused?
If a consumer refuses medication, it must be noted on the MARS by marking the corresponding hour with an "R" for Refused. This documentation helps healthcare providers understand the consumer's adherence to their medication regimen and can inform future treatment decisions.
Can the Medication Administration Record Sheet be modified?
While the basic structure of the MARS should remain intact for consistency, additional notes or comments can be added as necessary. Any changes to the medication regimen should be documented clearly, using the "C" for Changed symbol where applicable.
How often should the Medication Administration Record Sheet be updated?
The MARS should be updated each time a medication is administered. This includes recording refusals or changes. Regular updates ensure that all parties involved in the consumer's care have access to the most current information regarding medication administration.
Similar forms
The Medication Administration Record Sheet is an important document used in healthcare settings to track the administration of medications to patients. There are several other documents that serve similar purposes in ensuring proper medication management and patient safety. Below are seven such documents, each with a brief explanation of how they relate to the Medication Administration Record Sheet.
- Patient Medication List: This document provides a comprehensive list of all medications prescribed to a patient. Like the Medication Administration Record Sheet, it helps healthcare providers keep track of what medications a patient is taking and ensures that there are no harmful interactions.
- Prescription Order Form: This form is used by healthcare providers to prescribe medications. It is similar in that it outlines specific medications, dosages, and instructions for administration, which are later reflected in the Medication Administration Record Sheet.
- Medication Reconciliation Form: This document is used to ensure that a patient's medication lists are accurate and up-to-date during transitions of care. It shares the same goal of preventing medication errors, just like the Medication Administration Record Sheet does.
- Nursing Notes: Nurses document patient care and observations in these notes. They often reference the Medication Administration Record Sheet to confirm what medications were given, providing a complete picture of patient care.
- Incident Report: When a medication error occurs, an incident report is filed. This document is similar because it aims to improve safety and quality of care, addressing any discrepancies noted in the Medication Administration Record Sheet.
- Articles of Incorporation: Just as vital documents guide patient care, the PDF Documents Hub provides essential resources for completing the New York Articles of Incorporation, ensuring compliance with state regulations.
- Patient Care Plan: This plan outlines the overall treatment goals for a patient, including medication management. It relates to the Medication Administration Record Sheet by ensuring that all healthcare providers are aligned on medication administration strategies.
- Discharge Summary: Upon leaving a healthcare facility, patients receive a summary that includes their medication instructions. This document is similar as it reinforces the importance of the Medication Administration Record Sheet by providing continuity of care in medication management after discharge.
Guide to Filling Out Medication Administration Record Sheet
Filling out the Medication Administration Record Sheet is a straightforward process that ensures accurate documentation of medication administration. Following these steps will help you complete the form correctly and maintain a clear record of medication given to consumers.
- Begin by entering the Consumer Name at the top of the form.
- Next, write the name of the Attending Physician in the designated space.
- Indicate the Month and Year for which you are recording medication administration.
- For each day of the month, fill in the appropriate hour for medication administration in the corresponding box.
- If a medication was refused, mark the box with an R. If it was discontinued, use a D. For medications given at home, mark with an H. For those administered during a day program, use D, and if there was a change in medication, mark with a C.
- Ensure to record the time of administration clearly next to each entry.
By following these steps, you will ensure that the Medication Administration Record Sheet is filled out accurately, providing essential information for ongoing care and treatment.