Free Progress Notes PDF Form
Misconceptions
Many people have misconceptions about the Progress Notes form, which can lead to confusion and mistakes in medical record-keeping. Here are four common misunderstandings:
- Misconception 1: Progress Notes are only for doctors.
- Misconception 2: Progress Notes are optional.
- Misconception 3: Progress Notes only need to be filled out when there is a significant change in the patient’s condition.
- Misconception 4: Anyone can access Progress Notes without restrictions.
This is not true. While doctors often fill out these notes, any healthcare provider involved in a patient's care can document their observations and actions in the Progress Notes. This includes nurses, therapists, and other medical professionals.
In reality, Progress Notes are a crucial part of medical documentation. They help ensure continuity of care and are often required by regulations and insurance companies. Skipping this step can lead to gaps in patient care.
Progress Notes should be updated regularly, not just during significant changes. Routine updates provide a complete picture of the patient's ongoing care and can help identify trends over time.
This is a misconception. Access to Progress Notes is typically restricted to authorized personnel only, to protect patient privacy and comply with regulations like HIPAA. Unauthorized access can lead to serious legal consequences.
Documents used along the form
When managing patient care, several forms and documents complement the Progress Notes form. Each document serves a specific purpose and contributes to maintaining comprehensive medical records. Below is a list of commonly used documents.
- Patient Intake Form: This document collects essential information about the patient, including demographics, medical history, and current medications. It helps establish a baseline for care.
- Treatment Plan: This outlines the proposed course of treatment for the patient. It includes goals, interventions, and timelines, ensuring everyone involved understands the patient's care strategy.
- Employment Verification Form: This essential document confirms an individual's employment status, validated by various employment details. For further insights, you may refer to documentonline.org.
- Consent Form: This form secures the patient's permission for specific treatments or procedures. It ensures that patients are informed about the risks and benefits before proceeding.
- Referral Form: Used when a patient needs to see a specialist, this document provides necessary information about the patient's condition and the reason for the referral.
- Discharge Summary: This document summarizes the patient's treatment and progress during their stay. It includes follow-up care instructions and any necessary referrals.
- Medication Administration Record (MAR): This form tracks the administration of medications to patients. It ensures that medications are given as prescribed and helps prevent errors.
- Assessment Form: This document records the clinician's evaluation of the patient’s condition during each visit. It includes findings from physical exams and any relevant tests.
Utilizing these forms alongside the Progress Notes enhances the quality of patient care and ensures that all necessary information is documented accurately. Proper record-keeping is essential for effective communication among healthcare providers and for the continuity of care.
Check out Popular Documents
Facial Consent Form - Ensures your comfort level is prioritized during the treatment.
When engaging in the sale of a vehicle, it is important to properly document the transaction to prevent any misunderstandings between the buyer and seller. The Florida Motor Vehicle Bill of Sale form is designed to fulfill this purpose and serves as a vital record that confirms the sale and details essential information about the vehicle. To ensure you have the correct documentation, you can find the form here, which will help facilitate a smooth transfer of ownership.
Player Evaluation Form Basketball - Catch and shoot skills assess a player's readiness to score quickly.
How Long Does a Discharge Upgrade Take - Service members submit the DD 149 to the appropriate review board for evaluation.
Key Details about Progress Notes
What is the purpose of the Progress Notes form?
The Progress Notes form is used to document a patient's ongoing medical care. It helps healthcare providers keep track of a patient's condition, treatment, and any changes over time. This form is essential for maintaining accurate medical records.
Who should fill out the Progress Notes form?
Healthcare providers, including doctors, nurses, and therapists, are responsible for filling out the Progress Notes form. They should record their observations and any treatment provided during each patient visit.
What information is required on the Progress Notes form?
The form requires several key pieces of information, including:
- Patient's name (last, first, middle)
- Patient's grade, rank, or rate
- Hospital or medical facility name
- Patient's identification number
- Ward number
- Date of the entry
All this information helps ensure that the notes are correctly attributed to the right patient and visit.
How often should the Progress Notes form be completed?
The Progress Notes form should be completed during each patient visit or encounter. This ensures that all relevant information is recorded consistently and accurately over time.
Is there a specific format for writing Progress Notes?
While there is no strict format, notes should be clear and concise. Providers should focus on documenting the patient's condition, treatment provided, and any changes observed. Using standard abbreviations and medical terminology can help maintain clarity.
What should be done if there is not enough space on the form?
If the form does not provide enough space for detailed notes, providers can continue writing on the reverse side of the form. Alternatively, they may attach additional sheets if necessary. It is important to ensure that all relevant information is recorded.
How is the Progress Notes form used in patient care?
The Progress Notes form plays a crucial role in patient care. It allows healthcare providers to communicate effectively about a patient's condition and treatment. Other providers can review these notes to understand the patient's history and make informed decisions about future care.
Are Progress Notes forms confidential?
Yes, Progress Notes forms are considered confidential medical records. They should be stored securely and only shared with authorized personnel involved in the patient's care. Maintaining confidentiality is essential for protecting patient privacy.
What should be done if an error is made on the Progress Notes form?
If an error occurs, it should be corrected promptly. The provider should draw a line through the mistake, write the correct information, and initial the change. This method maintains a clear record of what was originally written while ensuring accuracy in the notes.
Similar forms
-
Patient Care Plan: Like Progress Notes, a Patient Care Plan outlines the patient's treatment goals and strategies. Both documents track the patient's progress and adjustments to care over time.
-
Clinical Summary: A Clinical Summary provides a comprehensive overview of a patient's medical history and treatment. Similar to Progress Notes, it documents significant events and changes in the patient's condition.
-
Discharge Summary: The Discharge Summary details a patient's treatment and progress during their stay. It is similar to Progress Notes in that it summarizes key information and recommendations for ongoing care.
Articles of Incorporation - This legal document is vital for establishing a corporation in New York, detailing key information such as name, purpose, and structure. To ensure compliance with state law, you can fill out the necessary form through PDF Documents Hub.
-
Referral Note: A Referral Note is used to communicate patient information when transferring care to another provider. Like Progress Notes, it includes important details about the patient's condition and treatment history.
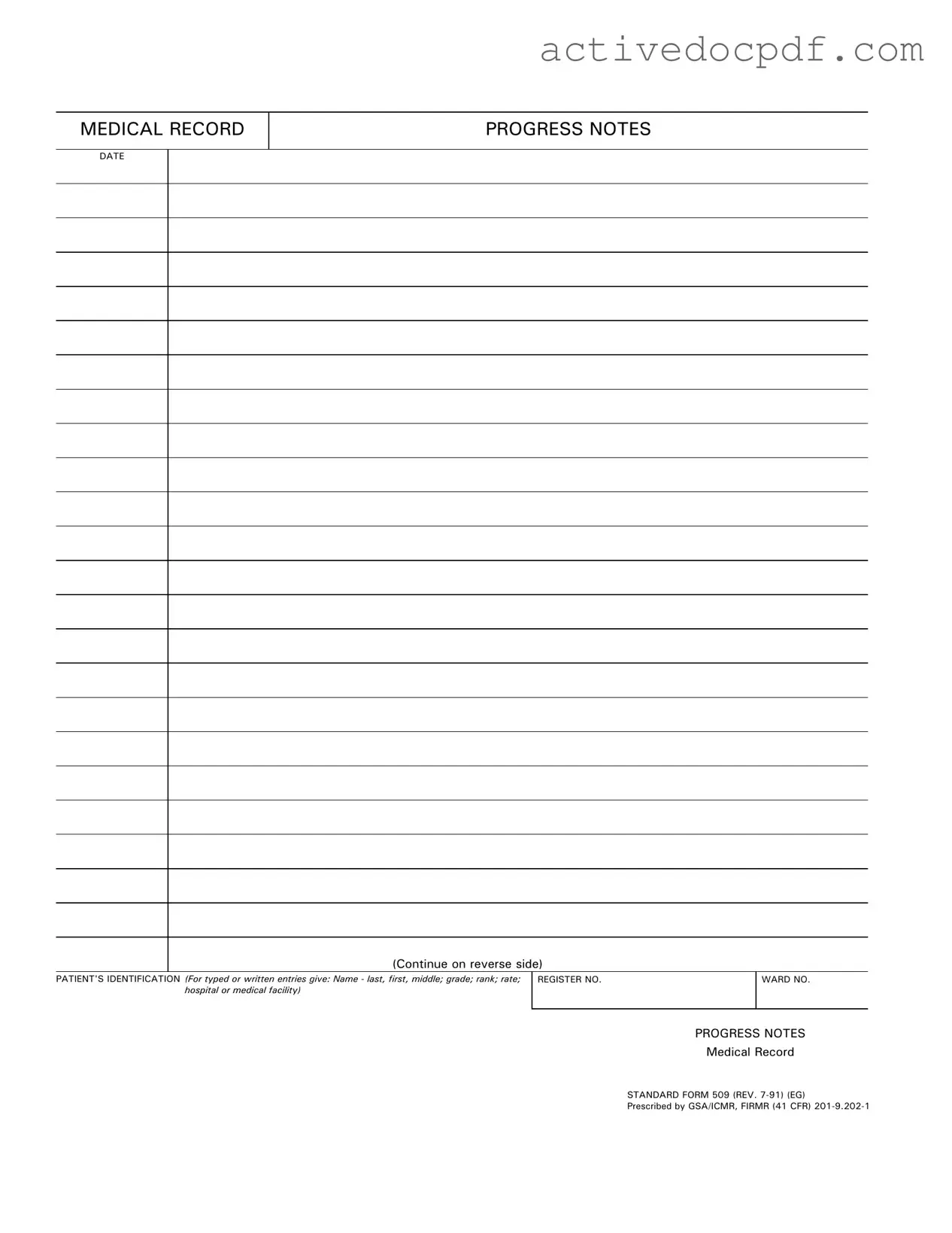
Guide to Filling Out Progress Notes
Once you have the Progress Notes form in front of you, it’s time to begin filling it out. This form is crucial for documenting a patient's medical history and ongoing care. Follow these steps carefully to ensure all necessary information is recorded accurately.
- Date: Start by entering the date at the top of the form. Use the format MM/DD/YYYY for clarity.
- Patient's Identification: Fill in the patient's name. Write the last name first, followed by the first name and middle initial if applicable.
- Grade, Rank, Rate: Include the patient's grade, rank, or rate, depending on their military or medical status.
- Hospital or Medical Facility: Specify the name of the hospital or medical facility where the patient is receiving care.
- Register Number: Enter the patient’s unique register number, which helps in identifying their medical records.
- Ward Number: If applicable, write down the ward number where the patient is being treated.
After completing these steps, review your entries for accuracy. Ensure that all required fields are filled out before submitting the form. This attention to detail is essential for maintaining clear and effective medical records.